The risk of lung cancer exists beyond smoking, as experts note that
NEWYou can now listen to Fox News articles!
Lung cancer, the second most common cancer in the United States, is often associated with smoking – but even those who have never had cigarettes could be at risk of deadly illness.
If it is true that those who smoke faces a much higher risk, up to 20% of lung cancers affect people who have never smoked or smoked less than 100 cigarettes during their lifetime, according to the centers for Disease Control and Prevention (CDC).
Despite this, the working group on the preventive services of the United States (USPSTF) does not recommend screening for lung cancer for those who have never smoked, as the agency indicates that the risks can prevail over potential advantages.
More toxic and carcinogenic disposable vapes than cigarettes, shows the study
Most lung cancers are divided into two groups: lung cancer non -small cells (NSCLC) and lung cancer with small cells (SCLC), according to the American Cancer Society.
The CBNPC, which includes around 80% to 85% of all lung cancers, includes adenocarcinoma (common in non-smokers), epidermoid carcinoma and large cell carcinoma.
Up to 20% of lung cancers affect people who have never smoked or smoked less than 100 cigarettes during their lifetime. (istock)
The remaining pulmonary cancers are classified as SCLC, a more aggressive type that tends to spread more quickly and has a lower prognosis.
Mohamed ABAZEED, MD, PH.D., ONCOLOGY RECOLIATION President and brand of brand William N. at the Northwestern University Feinberg School of Medicine in Chicago, applies that the share of lung cancers diagnosed in smokers to never increase, especially among women and Asian ascitch patients.
Cancer mortality rates decrease, but new diagnoses are increasing for certain groups, the report indicates
“Although the overall incidence decreases due to the reduction in smoking rates, the relative part of never smoking is developing and reflected in clinical practice, where we are increasingly diagnosing patients with no traditional smoking history,” he told Fox News Digital.
Dr. Lauren Nicola, an exercise radiologist and chief doctor of Reveal DX in Northern Carolina, said that she also found an increase in the newly diagnosed lung cancer in non-smokers, especially in women and young adults.

Most lung cancers are divided into two groups: lung cancer non -small cells (NSCLC) and lung cancer with small cells (SCLC), according to the American Cancer Society. (istock)
The main factor that increases the share of non-smokers in patients with lung cancer, according to Abazeed, is the desire to reduce tobacco consumption in the United States
“Other factors include improvements in imaging and wider use of CT scanners that have improved tumor detection at an early stage,” he noted.
“It is estimated that around 8% of lung cancers are inherited or occur due to a genetic predisposition.”
“The evolution of environmental factors can also contribute to this change, pollutants potentially leading pulmonary inflammation, which in turn was involved in the development of cancer.”
Modifiable risk factors
According to Abazeed, some of the largest non-smoking risk factors include ambient air pollution and secondary smoke.
Exposure to chest radiation (high energy radiation in the chest area) – as well as professional risks such as radon, asbestos and diesel exhaust – can also increase the risk.

The main factor that increases the share of non-smokers in patients with lung cancer is the desire to reduce tobacco consumption in the United States, according to experts. (istock)
Inflammation linked to lifestyle, which is often linked to poor diet and sedentary behavior, can also play a role, noted Nicola.
“Some of them, such as radon and air quality, can be treated in the household or policy,” said Abazeed.
Risks, symptoms and treatments for lung cancer, the deadliest cancer in the world
“Lifestyle interventions – such as exercise, diet and avoidance of interior pollutants – can play a modest protective role.”
The two doctors stressed that the former smokers, especially those who have smoked more often and for longer periods, remain high risks even decades after their stop.
“The higher the number of years of pack, the higher the risk,” said Nicola. “The risk decreases over time after leaving, but never comes back to the reference base of a smoker.”
Genetic risk factors
Some people inherit a higher risk of developing lung cancer because of their DNA.
“It is estimated that around 8% of lung cancers are inherited or occurred due to a genetic predisposition,” Abazeed told Fox News Digital.
Click here to obtain the Fox News app
“The inherited predisposition is an active field of investigation, especially in younger patients or those who have solid family history.”
According to Nicola.
“Up to 50% of all the chest CTS will detect at least one pulmonary nodule.”
“Non-smoking cancers are more often associated with specific genetic changes and genomic profiles,” she said. “This suggests that these malignant tumors have a different underlying biology from that of tumors in smokers.”
Projections in question
Current American screening lines call for low -dose annual computed tomography for high -risk individuals depending on age and smoking history, reiterated Abazeed.
The USPSTF recommends the screening for “adults aged 50 to 80 who have 20 history of smoking and who smoke or leave or leave in the past 15 years”.
Click here to register for our Health Newsletter
“There is an increasing interest in expanding the eligibility for the inclusion of non-smoking risk factors,” noted Abazeed. “Evidence accumulates that could potentially modify current directives at the population level.”
There are potential risks linked to the expansion of screening, according to experts, including the potential for overdiagnosis and false positives.
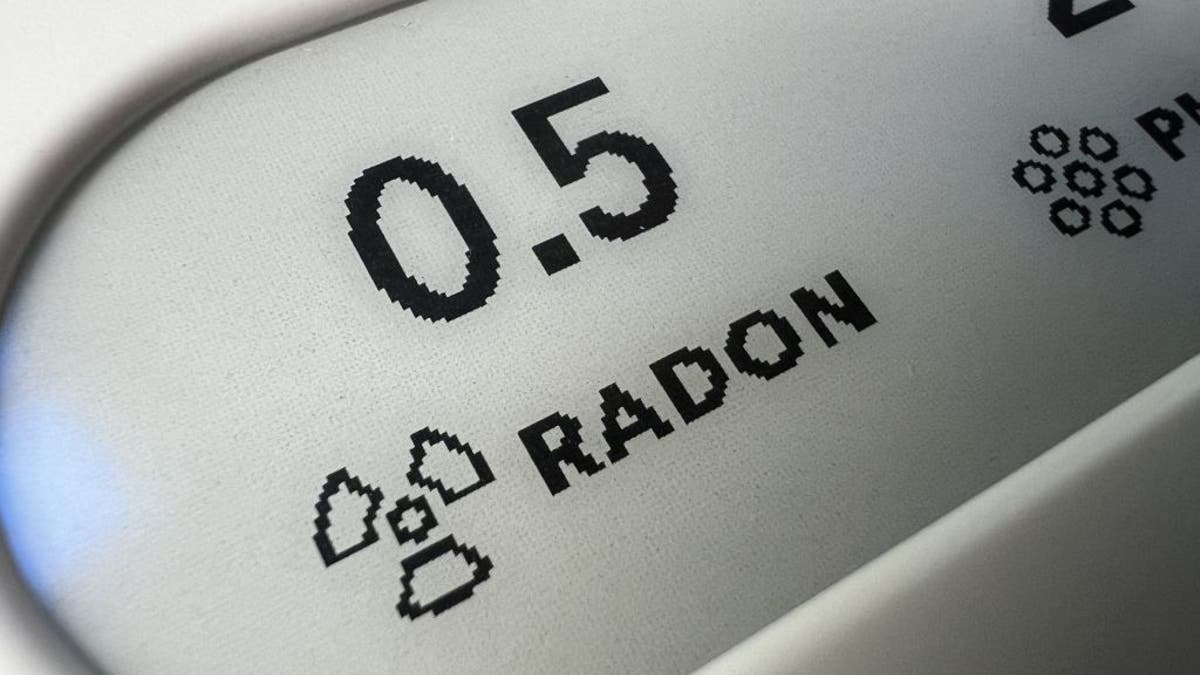
Exposure to professional risks such as radon, asbestos and diesel exhaust can increase the risk of lung cancer. (Photo of Gado / Getty Images)
“The problem with everyone’s screening for lung cancer is that up to 50% of all the chest CTS will detect at least one pulmonary nodule,” noted Nicola. “The vast majority of these nodules are mild, but a small percentage will prove to be cancer.”
Based mainly on the size of the nodule, the clinician can recommend follow -up imaging or biopsy.
For more health items, visit www.foxnews.com/health
“New tools are under development that can help us better characterize the risk of malignancy of a nodule, which will reduce the damage potential associated with a screening diagnosis,” said Nicola.



